As I gave Cindy her first hug of the day, claiming instead she was giving me a hug, I asked her the usual question: “Did you sleep OK.”
Back when Cindy could answer she always said “yes” even though I knew that could not be always true. I asked the question not so much to find out how she was sleeping, but to start the day with a dose of her innocent cheerfulness. I continue to ask the question in memory of that cheerfulness.

This morning I half expected an answer. The day before Cindy was alert and frequently smiled for both our morning visitor and our afternoon home health aide. Such alertness is typical for two days after a seizure.
Since Cindy’s first seizure in March 2019 she has averaged about one a month. Sometimes they are weeks apart, sometimes months. The day following a seizure Cindy spends more time than usual resting. Then the next day, no matter how severe or mild was the seizure, Cindy shows greater clarity and good humor.
Since Cindy has been in hospice care I give her a small dose of lorazepam, included in the hospice package, when she becomes “twitchy (there are commonalities between Alzheimer’s and Parkinson’s).” Occasionally, I will give her lorazepam before bedtime to increase the odds we will sleep through the night. That was before I rediscovered that anti-anxiety drugs increase the chances of dementia, or possibly an earlier death from dementia.
I had skipped the lorazepam for a couple days before this latest seizure, even though there were a couple signs that the next seizure might occur. She was twitchy in the evening ; she did not have a bowel movement for a couple of days. When the seizure occurred I did not kick myself, but rather became hopeful for what might happen next.
I was not disappointed as she smiled frequently for both our visitor and home health aide. As I was taking Cindy’s socks off that evening I got the inspiration to play “This little piggy” with her. She cracked a pleasant smile as I went “wee, wee, wee all the way home.”
The next morning Cindy again flashed a couple of smiles, though not as many. As the day progressed she reverted to the norm. During our evening “dance” my now impassive partner got my sleeve and arm soaked with drool. A seizure can buy a couple days of alertness and humor, but not more.
This now is my biggest dilemma as a caregiver. Do I give lorazepam only after a seizure? If I do that she will have better brain health and longevity, more moments of joy. Or do I give lorazepam whenever the signs are there for a possible seizure? That means more sleep for me, less discomfort for Cindy.
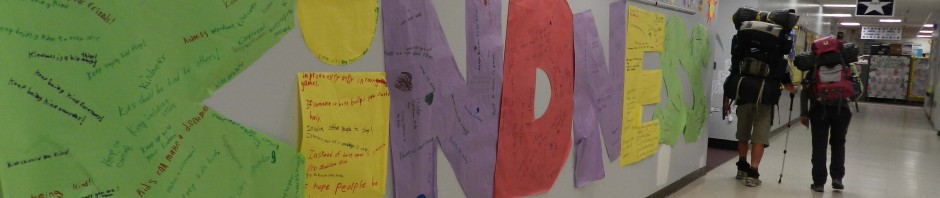
I suspect most people would do everything to make a loved one comfortable in the present. Yet as long distance backpackers both of us are accustomed to discomfort as a necessary byproduct of a preferred lifestyle. If I were in Cindy’s shoes I would opt for joy over comfort. I have no doubt that is Cindy’s preference as well.
It ain’t easy watching your loved one twitch almost to the point of convulsion. It’s even worse when the convulsions start. On the other hand, my greatest moments of joy these days as a 24/7 caregiver are Cindy’s moments of joy. I fear there would be no joy left in her, plus I could be hastening her demise, if I relied too heavily on lorazepam (which actually is one of the most harmless anti-anxiety medicines).
I do use other means first to reduce twitching. I give Cindy supplements like melatonin and ashwagandha to calm the mind. I play guitar and sing for her. I read to her. We go out for long jaunts in the stroller. She never gets twitchy during one of our jaunts. Yet these strategies cannot be maintained constantly throughout a day. Giving her lorazepam every time she twitched would still amount to a couple times a day.
What a dilemma! Given the state of constant decline, no doubt I will have to give her lorazepam frequently. Did I mention that morphine also is in the hospice package? For now that’s a dirty word, an unthinkable. Ironically, if/when the situation gets to that point I can be assured that she will have slept OK, but the cheerfulness that Cindy embodies will be gone.
I vote ‘joy over comfort.’
Kirk….I believe you are doing the right thing. You have done right all along. Love is THE most important healer. Letting her have joy is again so important. Are you at all aware of what is happening on an earth scale? If Cindy is an empath, she has been in hell. Many of us are having experiences like hers. We have declined diagnosis and are fighting with all we have to get to the other side. We are getting there. I know you read this and say, but you are cognizant, Peggy. Yes, I am. I can write what I feel which helps a lot. I know also what is happening to the earth and solar system, which helps to keep me out of fear, even though what is happening has never happened before. The human race is surviving this time. As a solar system we are moving through a new part of space, some call it the Photon Belt. We are being exposed to photon energy which will penetrate bodies and brains and hearts and make them adapt. Empaths are having the worst adjustment time, because they absorb everything.adapting for us is a huge challenge. I would guess that Cindy was exposed early on, maybe due to higher altitude climbs? I don’t know. And because of the history in your family she was diagnosed with Alzheimer’s. And the fear factor kicked in. Fear is our worst enemy. Lucky for Cindy, you continued the Love, which can counter act fear and eventually help heal.
You may or may not believe me, Kirk. Very few do. But there are others, and thousands of us, who are very aware of what is happening. The focus on ascension was an unfortunate misnomer because it indicates a religious happening. It is not. Our consciousness is changing and becoming of a higher frequency, which equates to Love. There is a lot of info now written about energy changes and symptoms. And our bodies and brains are changing and adapting. I don’t know where to start you, but I think you might now believe what I tried to tell you years ago.
BTW I live with but have no intimate connection to a man who is experiencing this through his creativity, like you. He can’t stop creating and is loving it. Only those of us who spent our lives giving to others, we are having a rough time. I guess others are feeling it in different ways. Many bodies are very sick. Some leave. Politicians are having the challenge of a lifetime. It is all connected to these changes. Really.
Peggy
In the last long vigil there comes a time when the most loving thing we can do is tell them we love them, we will miss them, but give them permission to leave us.
There’s hardly ever a black-and-white answer that satisfies – hence the dilemma. I love you both very much and trust that you’ll communicate with each other toward a good balance of both comfort and joy. In the meantime, I count myself as blessed for the opportunities I have to visit and share both joy and comfort – sounds like a recipe for peace.
We appreciate your regular visitations. You are a highlight to the week.
A joyful moment may minimize discomfort!!